Every other Friday morning during the academic year, a small group of Seattle Pacific undergraduate and graduate students gathers in a classroom in Demaray Hall.
They come from a variety of disciplines: psychology, nursing, marriage and family therapy, theology. But they join to learn, study, listen, and dialogue with one goal relevant to all of their fields and future careers: understanding and serving individuals and families affected by severe mental illnesses.
These students are part of the Dickinson Fellowship, a one-year interdisciplinary program at Seattle Pacific that provides funding and training for eight students each year in the area of mental health through readings and discussions, conferences, guest lecturers from around the nation, service opportunities, and field experience. The fellowship is part of the Living Well Initiative, which sponsors community outreach and research related to mental illness, community health, and faith.
“Dickinson fellows are the health care workers, nurses, psychologists, church workers, and counselors of the future,” said Paul Kim, associate professor of psychology and one of the faculty scholars for the Dickinson Fellowship. “They’re learning how to best serve those struggling with mental illness and combat the surrounding stigma.”
Case in point: Candice Xia ’18, a bright, cheerful nurse passionate about serving mental health patients. Xia completed the Dickinson Fellowship while studying nursing at SPU.
“The fellowship challenged me to build relationships with people who are struggling with mental health.” —Candice Xia
After graduating, she was hired as a registered nurse for International Community Health Services, a nonprofit clinic in Seattle. The clinic provides primary care to people who often do not have adequate access to health care, including immigrants, low-income families, uninsured individuals, and people experiencing homelessness. Many patients have mental illnesses, and the clinic either treats them or refers them to more specialized resources.
“The fellowship challenged me to build relationships with people who are struggling with mental health,” said Xia. “Now as a nurse, I feel prepared to initiate those relationships.” Xia’s patients often come to the clinic describing physical problems, but after she builds a relationship with them, they share mental health concerns and she connects them with resources.
Treatment gap
Nurses like Xia fill a large gap in health care.
Nearly one in five adults in the U.S. — 44.7 million in 2016 — lives with a mental illness, but more than half of them don’t receive treatment, according to data from the Substance Abuse and Mental Health Services Administration and Mental Health America.
Outside the U.S., the treatment gap is even larger. The World Health Organization estimates that more than 450 million people worldwide suffer from mental illness, but as many as 85 percent in low- and middle-income countries receive no form of care.
Common misconceptions and stigma surrounding mental health perpetuate the treatment gap. Gretchen Hawkins, a mental health advocate and former board member for the National Alliance on Mental Illness who now is a regular guest lecturer in the Dickinson program, says the main culprit is lack of education.
“People often treat mental illness as a moral or character weakness that you could overcome, instead of a medical disorder…” — Gretchen Hawkins
“People often treat mental illness as a moral or character weakness that you could overcome, instead of a medical disorder,” she said. “But just like there’s a proper response to someone having a heart attack, there are proper responses to mental illness that people need to learn. Because when we don’t understand, we fear and judge.”
Hawkins knows firsthand the fear that individuals with mental illness encounter. More than a decade ago, she found herself standing in an empty one-bedroom apartment in Seattle after a sudden feeling of omnipotence and divine intervention moved her to sell her possessions and leave her previous home where she had lived with her two sons.
When she realized what she had done, she went to Harborview Medical Center, where she was diagnosed with bipolar 1 disorder. Distanced by her family and friends, she endured the long journey of reaching stability without that social network.
Today Hawkins thinks that personal stories are some of the most powerful tools to reduce the stigma around mental illness.
Today Hawkins thinks that personal stories are some of the most powerful tools to reduce the stigma around mental illness. She presents her story for “In Our Own Voice,” a program where people living with mental illness pair up to discuss their experiences in schools, churches, businesses, and elsewhere.
Xia agrees. “Learning about people’s stories changed my heart,” she said. “I stopped seeing them as their diagnoses, and instead saw them as people with families and struggles, like me.”
Family impact
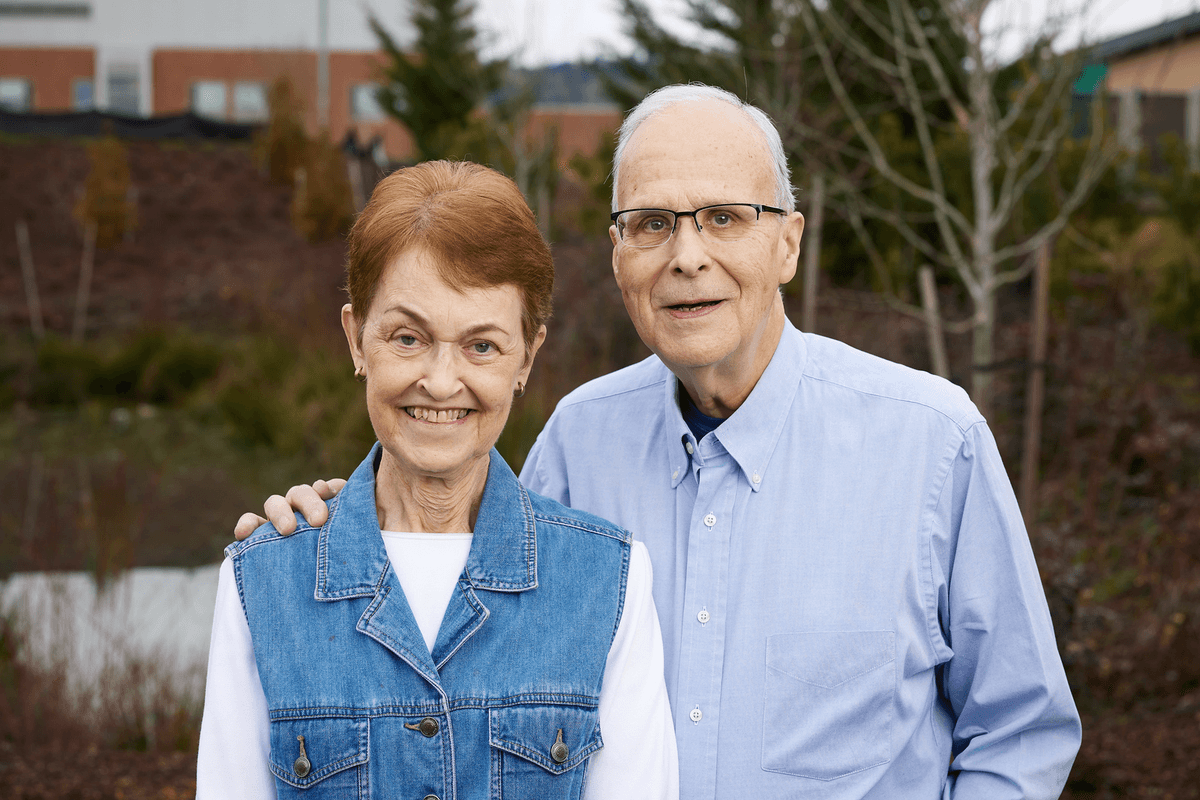
The Dickinson Fellowship began with Lew and Jackie Dickinson, a couple whose son, Luke, was diagnosed with schizophrenia just weeks into his sophomore year at Seattle Pacific. In the autumn of 1991, Luke — an excellent student, promising hockey player, and dependable friend and employee — experienced a mental health episode and was hospitalized.
From their home in Alaska and with the demands of their family business, Lew and Jackie felt far away and helpless. But even though Luke dropped out of school, several SPU staff members supported him as he adjusted to life with a severe mental illness.
The Dickinsons knew that many families of people with mental disorders did not find this kind of support. In 2002, to raise healthy awareness of mental illness and equip students to be effective caretakers and advocates, the family established the Living Well Initiative. The initiative is co-sponsored by SPU’s School of Health Sciences and School of Psychology, Family, and Community. The family provides annual program gifts and also established an endowment in 2014 to ensure ongoing funding for the program.
“By ourselves, we could only help a handful of people,” said Lew Dickinson. “When we invest in students, they will help someone else, and then they will help someone else. It’s gone way beyond what we expected.”
“Every time I speak with these students, I sense quiet, unspoken compassion, love, and understanding.” —Gretchen Hawkins
Hawkins is the program director for Seattle Clubhouse, a social/vocational rehabilitation center for individuals with mental illness, and has been a guest speaker for SPU for the past seven years. She said that Dickinson fellows are great examples of what happens when educated Christians focus on mental illness.
“Every time I speak with these students, I sense quiet, unspoken compassion, love, and understanding,” she said. “They are quick to listen.”
Dickinson fellows are intentional about being supportive and present with those they interact with — a critical quality for future health care leaders, she added.
Learning in the classroom and the field
Listening to the stories of individuals with mental illness plays a key role in the Dickinson Fellowship curriculum. During Autumn Quarter, students dive into the memoirs and stories of individuals with mental illnesses, ranging from depression and severe anxiety to bipolar disorder and schizophrenia to substance abuse-related conditions. Winter Quarter, students study how mental illness affects the families of patients and the community at large. Finally, in Spring Quarter, fellows study advocacy and, in light of what they’ve learned, ways to advocate for those with mental illnesses.
Over the course of the program, relationships and cross-disciplinary connections are key as students bring questions and insight from their different fields to the table.
“I’m used to talking in terms of theology,” said Brent Watson, a 2018 Dickinson fellow and Seattle Pacific Seminary graduate who now works as a medical chaplain at Harborview Medical Center in Seattle. “It’s helpful to talk with people who are working with these populations in other ways. Everything you are affects your mental illness and how it’s manifested, so a holistic approach is important.”
“It’s helpful to talk with people who are working with these populations in other ways. Everything you are affects your mental illness and how it’s manifested, so a holistic approach is important.” —Brent Watson
The program also emphasizes relationship building with patients. Xia recalls a psychiatric ward visit during her training. She was not given the patients’ charts before meeting and interacting with them. She was nervous at first, because she knew the patients had been involuntarily admitted and would be very sick.
But a patient sitting at a table invited Xia to play checkers with her, and soon another patient joined them. “It felt like I was playing a game with friends,” Xia said. “Afterwards, I read their charts, and understood why they behaved certain ways. But since I didn’t know their diagnoses at first, I got to know them as people, and just listen to their stories.”
Xia grew up in China, where she said mental illness is rarely discussed, and discussing cultural differences with fellows from Singapore, Colombia, and the U.S. helped them broaden one another’s knowledge of cultural approaches to mental health.
“Patients don’t have just physical needs. They have psychological, social, and spiritual needs too,” said Xia. “I’ve gotten to see students with different experiences and perspectives come together on one topic.”
These discussions propel fellows to learn and serve outside the classroom. As part of the program, they observe King County mental health and drug court sessions, witnessing firsthand and analyzing how the law and mental health treatments come together.
Dickinson fellows are surrounded by a population that is especially at risk of mental illness: college students.
Undergraduate fellows lead SPU’s National Alliance on Mental Illness club, planning quarterly events on campus to foster understanding of mental illness. Last year, the club hosted a panel on the intersection of mental health and faith, as well as the Depressed Cake Shop, a bake sale raising mental health awareness, with all proceeds supporting the Seattle chapter of the National Alliance on Mental Illness.
Raising awareness
Dickinson fellows are surrounded by a population that is especially at risk of mental illness: college students. People are often first diagnosed with mental illnesses between the ages of 18 and 20, said Hawkins. According to a 2017 American College Health Association survey, 40 percent of college students said they felt so depressed that it was difficult for them to function, and 61 percent reported feeling overwhelming anxiety. The percentage of students visiting counseling centers has risen over the last decade, according to the Center for Collegiate Mental Health.
Last spring, prompted partly by this growing awareness of mental illness among college students, Dickinson fellows sent out a campuswide call for students to anonymously share their own experiences. They also asked students to share what gave them hope, and what they wished the SPU community understood about mental health disorders.
Stories poured in about students battling mental illness, or supporting loved ones through mental health struggles, and were displayed on a wall of the Student Union Building throughout May, nationally recognized as Mental Health Awareness Month.
The interdisciplinary nature of the Dickinson Fellowship is unusual among higher education mental health programs because of the way it blends faith, medicine, and community involvement, said Lorie Wild, dean of the School of Health Sciences. Wild co-administers the fellowship with Katy Tangenberg, dean of the School of Psychology, Family, and Community.
“Since I didn’t know their diagnoses at first, I got to know them as people, and just listen to their stories.” —Candace Xia
For Xia, the most challenging part of the fellowship was realizing how much work is left to be done in building support systems for those who struggle with mental illness and raising healthy awareness of the issue.
“It can be discouraging,” she said. “But we finished knowing we need to continue fighting for these people wherever we end up working, and share what we learned with everyone we encounter.”
Tools of the faith
The Christian church has not always handled the topic of mental illness well. According to a 2014 survey by LifeWay Research, more than half of Protestant senior pastors mention mental illness to their congregations no more than once a year. Only about one-quarter of churches surveyed had a system to assist individuals with mental illnesses or their families. And even when churches had mental health resources on file, nearly three-quarters of congregants did not know those resources existed.
“Christians are especially prone to thinking that mental illness is a moral or spiritual failing, rather than a chemical imbalance.” —Brent Watson
This lack of conversation and resources can exacerbate misconceptions. For instance, Christians are especially prone to thinking that mental illness is a moral or spiritual failing, rather than a chemical imbalance, said Watson, the Harborview chaplain.
And this is where programs like the Dickinson Fellowship contribute to the health of the church — and the world. By combining a strong understanding of faith with understanding of the biology of mental illness, graduates of the program are equipped to speak and work in a field in need of compassionate, informed caregivers.
“The tools needed to care for people with mental illness — inclusion, patience, love, kindness, attention to people who are ignored — are inherent to our faith,” Watson said. “All we have to do is rediscover and exercise them.”
Dickinson fellows are putting these tools to use. Since its genesis 16 years ago, 148 students have completed the Dickinson Fellowship. They now serve as psychologists, therapists, counselors, nurses, researchers, and doctors across the nation.
“Whether they are working directly with mental health patients or not, these experiences and lessons in communication, compassion, and understanding will always be with them,” said Wild. “Everybody has mental health issues — just in varying degrees.”